Me
@mattdoc1988
Followers
1,314
Following
2,885
Media
749
Statuses
6,973
Intensive Care Medicine & Anaesthesia Consultant. Married to cycling, running, holidays & wife (any order). @thepoppystudy coinvestigator
Devon, South West, England
Joined December 2015
Don't wanna be here?
Send us removal request.
Explore trending content on Musk Viewer
Elon Musk
• 471407 Tweets
Champions
• 378502 Tweets
Alexandre de Moraes
• 361952 Tweets
Brazil
• 349956 Tweets
Se o Twitter
• 317584 Tweets
Colorado
• 264759 Tweets
Mbappe
• 224452 Tweets
لاس بالماس
• 195862 Tweets
Real Madrid
• 184778 Tweets
Beşiktaş
• 177815 Tweets
Xandão
• 102218 Tweets
Bluesky
• 77522 Tweets
Hermoso
• 70874 Tweets
McDonald
• 67159 Tweets
Kutlu Olsun
• 67072 Tweets
Mustafa Kemal Atatürk
• 59866 Tweets
#BJKvLUG
• 54141 Tweets
#الاتحاد_التعاون
• 53963 Tweets
كاراسكو
• 47524 Tweets
Vini
• 38466 Tweets
#30AgustosZaferBayramı
• 35944 Tweets
LIBERTÁ IS OUT
• 32761 Tweets
Amrabat
• 29534 Tweets
Rafa Silva
• 29418 Tweets
Brahim
• 21896 Tweets
Servette
• 21512 Tweets
避難指示
• 20933 Tweets
Ancelotti
• 20930 Tweets
Tchouameni
• 19020 Tweets
#خلصوا_باكايوكو_للهلال
• 18900 Tweets
緊急速報
• 17771 Tweets
Modric
• 16681 Tweets
Kroos
• 16246 Tweets
Abdullah Avcı
• 12575 Tweets
Jack White
• 12007 Tweets
多摩川氾濫
• 11580 Tweets
Valverde
• 10868 Tweets
Mendy
• 10128 Tweets
Last Seen Profiles
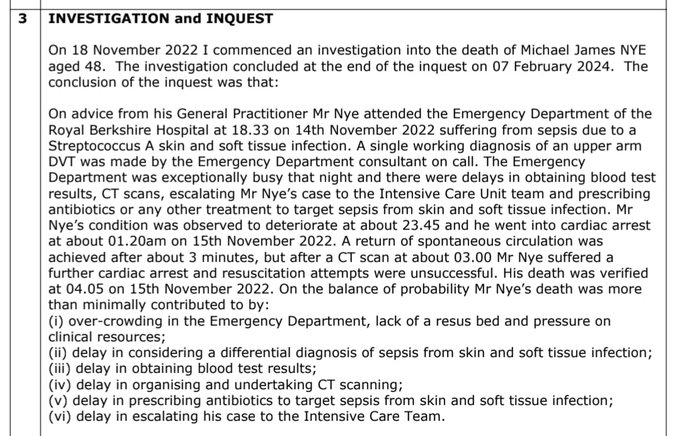
The reality of Intensive Care at the moment…
A Covid patient admitted to ICU means another patient cannot have their brain tumour operated on or their stomach cancer removed.
It’s one patient in, one patient out.
Some Covid admissions are avoidable.
#GetVaccinated
21
437
2K
@LozzaFox
Pertussis is whooping cough, a bacterial lung infection. The reason you haven’t heard of it is because we are vaccinated against it in childhood. Therefore, you are not aware of people suffering from pertussis. Which is the whole point of vaccines.
8
2
199
‘Interesting’ case.
Dementia, significant sacral sore, NH resident.
Resources used:
CT head
CT abdo/pelvis
MRI head
Abdo USS
EEG
ICU stay with I&V
Apart from anything else, where is the dignity in dying & pragmatism in end of life care?
17
7
154
@berger_nicky
@HorsleyCarl
Unfortunately life doesn’t work like that. That would mean no one should ever make a mistake. Systems, especially in healthcare, are complex. Many opportunities of errors to occur. We try to reduce these but it’ll never be completely error free unfortunately.
3
1
123
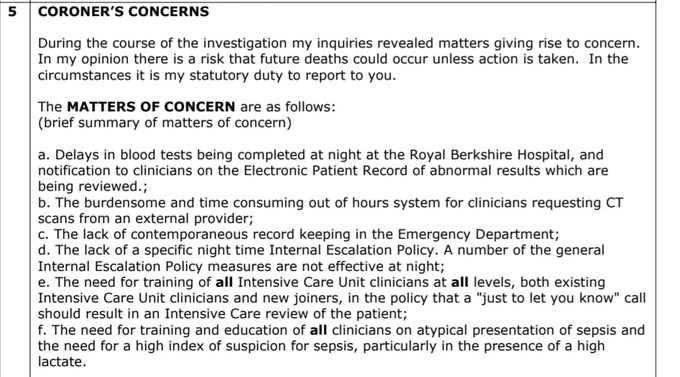
Coroner’s report stating all ICU referrals saying “just to let you know” should result in an in person review of the patient.
🚨 The
@RBNHSFT
A&E seems risky out of hours! Coroner says overcrowding in A&E was one factor that contributed to a man's death...
28
103
232
31
21
113
@nikosevangelou3
Sorry to get nerdy but it’s actually nitrous oxide (N2O).
Not nitric oxide (NO).
🤓
4
3
111
To all doctor colleagues. I think we should all back
@Jeremy_Hunt
as Tory leader. He's supported us so much recently I thought it'd be nice.
4
58
80
Moet in the fridge for this evening.
Passed
#FFICM
MCQ 🥳
Now just need to think about this viva/OSCE. Any tips?
#theendofexamsisinsight
#moetmedic
3
0
73
@aroradrn
My wife’s grandmother (from Thailand) reheats cooked rice on the wall in the sun in the back yard. 😮
She’s doing very well still!
1
0
67
I’ve been fast bleeped to NICU for airway difficulties on a few occasions as anaesthetic SpR. Also managing collapsed neonate in ED.
NICU have v different approach to airway management - I have never come across in any other clinical practice (inc adult & paeds anaesth & ICM)
@thatsnotmine125
@VirtueOfNothing
@telswood
@Matt_L_Nash
This does seem a bizarre conversation
Intubation of the critically ill adult is rife with risk & complications. Harm is common.
Intubation of the neonate (especially when critically ill) is a league up in failure, delay & complications. Harm is intrinsically less easy to
12
51
311
9
5
61
@SteveBarclay
@BMA_JuniorDocs
Your door is as open? Well then just start talking to the BMA then rather than playing politics.
0
2
60
@JonBall
If you pave that close around a tree that size then you’re going to kill the roots. Fairly predictable. Who designs pavements like that?!
2
1
51
A challenging case that highlights the risks of giving sedation in an acutely unwell patient with obesity in difficult circumstances.
A 38-year-old black man died at
@NHSBartsHealth
after a flawed decision to sedate him. Coroner criticises "coping culture" and the trust response including governance failures and poor effort by lawyers
#patientsafety
51
170
373
8
3
53
@Iromg
@LoftheBridge1
You can’t train to be a consultant in private hospitals. So juniors doctors don’t work in private hospitals. We have to work for the NHS.
3
1
45
@when_cats_away
@LeeHurstComic
Thanks. Even in the middle of a pandemic people can’t be nice to others. NHS staff really appreciate your feedback. 🙄
1
0
44
@jon1467
A 4th year med student, having spent a day in theatre, once asked a consultant anaesthetist “What do anaesthetists actually do?”
8
0
35
@SteveBarclay
You make it sound like you’re giving it to them willingly. They did go on strike to get that from you!
0
1
31
@tombircher
Or they could be cared for in special beds inside rooms, looked after by doctors and nurses called…
Helping Old & Sick Patients Inorder To Alliviate iLlnesses
Just a thought. Especially, given winter pressures. 🤷♂️
1
0
31
Amazing support from Consultants at Royal Devon & Exeter Hospital for
#juniordoctors
.
@TheBMA
@johannmalawana
0
29
27
@DGlaucomflecken
@DrEricStrong
@CaseMcQuade
I’m pretty sure the stroke doctors do something about strokes occasionally.
1
0
30
@DrRJWebb
It definitely exists. Grossly oedematous but any hint of diuresis they become hypotensive and/or hypernatraemic.
My approach is…
1 do they need diuresis. Can they do it themselves?
2 go gentle - low dose with a combination of diuretics (furosemide, spironolactone, metolazone)
2
0
29
@PictonChris
@RoyalAdelHosp
@SteveBarclay
@RishiSunak
- sponsoring the Australian health system.
#NHS
@NadineDorries
- maybe think about what other systems are doing right/better before trapping doctors in NHS.
0
2
27
Copy of
@BJAJournals
arrived in post today. Couldn’t help noticing, whilst the Anaesthetist & ODP are calmly inserting a cannula, the patient’s oxygen sats appear to be 79%. Arm doesn’t look hypoxic though I guess.
8
0
29
@David_Cameron
@Jeremy_Hunt
Seems like ur example of uniform 7 day elective work at
@SalfordRoyalNHS
isn't true.
4
65
27
@EmergMedDr
@CdoggMiller
@VictoriaLIVE
So he’s done F1/2. How does that make him a ‘junior surgical doctor’? That means I’m a junior surgical doctor too! Snap! He probably did one surgical job once during F1. What’s more important is if he’s done Obs & Gynae really. They’re the ones that do abortions, not surgeons.
1
2
25
@PBSherren
Always seems to be the people that are most vulnerable to Covid, and most likely to get severe Covid, that would benefit the most for wearing a face mask but are ‘exempt’… 🤷♂️
“My severe asthma stops me wearing a face mask”.
2
0
27
@Resuspiece
In addition, my real bugbear (initially) of not giving contrast for CTs in unwell patients because of ‘the kidneys’.
1
0
27
These comments are not helpful. You can’t quote 97% mortality in ventilated Covid pts and then paste the reference as a range 81-97%. And completely ignore the early UK
@ICNARC
data. All data sets are small. Also, UK ICU admission criteria often v different.
Scares the public.
Why is everyone so caught up in the ventilator love myth?
If you get put on mechanical ventilation, you have about a 97.8% chance of dying.
Yes we need lots of ventilators.
No, they will not prevent the vast majority from dying.
#Covid_19
38
53
270
2
1
26
I find it odd as an ICM trainee I have had no further training in breaking bad news or difficult conversations since I left med school.
Today I watched 10 doctors try to have a DNACPR discussion in the context of discussing a deteriorating patient.
Even those most skilled in communication made the task so much more difficult that it needed to be.
@DrLindaDykes
we need to sort this out
⬇️
42
147
460
9
4
26
@IM_Crit_
But would you let a patient choose a chemotherapy that had no benefit for their cancer?
Or an antibiotic that we knew their infection was resistant to?
Why is CPR different?
3
2
25
@IM_Crit_
200 beds would be a pretty small hospital in the UK!
All ICUs staffed by intensivists but some smaller ones share oncall rota with anaesthesia.
I guess the geography of UK is very different to the US.
3
0
24
@WelshGasDoc
Oh no, I’m about to be very ill.... I need to drive somewhere! 🧐
Maybe need to look at
@DVLAgovuk
regulations?
0
1
22
If only there was a 5-6 year lead in time for the UKFPO to prepare for the graduation of these med students….
🤔
0
3
24
SHO doctor rota gaps in Emergency Dept in hosp near me
#mindtherotagap
@Jeremy_Hunt
@HackneyAbbott
@sarahwollaston
7
57
22
@_skylined_
Kate. I’m so sorry you are going through this. (Slightly depends on individual hospitals) but there is often support for post-ICU patients. Follow up clinics where you can seek help with understanding what you’ve gone through. They can link into psychological support.
0
0
23
@Jeremy_Hunt
I've already sent u 2 invites to shadow me at work. Still haven't heard back. I'm getting quite upset now Jeremy. Please RSVP.
2
16
21
Having an NSAID around the time of endurance exercise could be dangerous.
Voltarol is sponsoring the London Marathon!
Someone think of the kidneys!!!
2
2
21
This is really great idea for
@wesstreeting
A central library of NHS guidelines (both local and national).
Why have 1000s of separate guidelines for each hospital across the UK when we could share many (or at least make minor local amendments).
3
2
18
@Med_Registrar
Don’t think I’ve ever asked the medics to attend in person. But needs to be really clear what samples need sending and how.
0
0
19
@drokane
This is quite old school. However, I think it’s important a consultant/senior doc should be involved in the original referral & then needs to be discussed with ICU consultant regardless. The more complex the patient there definitely should be consultant to consultant discussions
3
0
20
@doctorrxg
@ICU_Management
We do offer ‘treatment’ - antibiotics, draining infections, anti-epileptics, etc.
But ECMO, ventilation strategies are not treatments. They temporise things. They don’t effect the underlying disease. They prevent lung injury and allow time for recovery & allow Abx to work.
2
2
19
@Microbedoc2
I do think switchboards should have a statement for each specialty overnight.
“This specialty has a 24hr on call. Are you sure you want me to put you through?”
Or non-resident oncalls should be slightly protected between say 2am-6am with switch checking it’s a true emergency.
2
2
20
@iainpdooley
@fhussain73
@NHSEngland
@rankinphoto
The vaccine is not compulsory. No one is making anyone have the vaccine against their will. However, there is a lot of misinformation out there and some apathy so a gentle nudge from your trusted GP may change a few people’s minds. Excellent work
@fhussain73
2
0
18
@johnestevens
Sounds a very sensible idea. As long as people satisfy the set criteria they can have it. It’s technically very easy to administer.
0
0
18
@ncl_medic
@guardian
This is why it’s not called brainstem death! Should be called ‘death by neurological criteria’.
It’s a confusing concept for medics/lawyers… let alone grieving parents! So we should keep it as simple as possible: “he has died”.
1
0
18
@cindylou12
@ReevePara
@Danielf90
Usually on ICU we put them in the ‘superman’ position with one arm in front crawl position and head to one side on a pillow.
There are many proning contractions we normally use in theatre for e.g. spinal surgery but not usually appropriate for ICU.
0
2
18
I get the feeling
@NHSE_WTE
must have said a few years ago that specific courses (inc ALS/ATLS etc) should no longer be compulsory on training curriculum - to save them £££ in their study budgets.
🧵
1
1
18
Everything that is wrong with medicine - the system is set up to act contrary to the best interests of the patient.
Some of the most rewarding & meaningful times in medicine are doing less: not giving a medication, not performing an operation, not admitting to ICU….
1/2
2
3
18
Please please please just stop spouting lies and concentrate on sorting out this mess. Stop spinning. Infuriating.
.
@Jeremy_Hunt
: the resumption of talks shows the Govt’s door is & has always been open to meaningful talks
#HealthQuestions
#JuniorContract
135
4
1
0
18
15
@DrHoenderkamp
@DocAnonX
@DianaBlackburne
@drdavidbull
@prema14
Renee, if you could detail the tuition fees you paid when you went to medical school?
Students now pay £9000/year to study medicine. It’s not free or paid for by government. It’s subsidised but certainly not free.
1
0
17
@Jdon101_
When I did an ED job, I wished something existed for ED docs similar reasons. Would be SO educational to get that feedback. We had access to discharge summaries so I would save some hospital numbers & look them up on a quiet shift.
0
0
18
@JackBarton07
Functional/social history really important. No one ever documents it again after admission but it’s key for ICU reviews. Gives an idea of physiological reserve. Keep it simple - can they climb flight of stairs, walking distance, do own shopping/ADL, occupation, driver… ?
2
0
17
@TurtonsOther
@MedCrisis
I had an ICU sister once tell me to “leave the unit and go to bed” because there was nothing to do! 🤩
0
0
17
@rupert_pearse
Do you have data on ICU & hospital admissions and the patients’ vaccine status? Can’t seem to find this info easily?
3
0
17