Craig Tschautscher
@TschautscherMD
Followers
519
Following
3K
Statuses
907
UW Flight and EM/EMS doc, opinions are my own.🇩🇪 🇺🇸
Madison, WI
Joined March 2017
RT @MadtownEM: Badger family photos from #NAEMSP2025 ❤️🦡 @UWEmerMed @UWMedFlight @NAEMSP @WINAEMSP @TschautscherMD
0
2
0
RT @UWEmerMed: The kind of energy we bring to the function 😁 We've had a great time at #NAEMSP2025, and are proud of the work we presente…
0
5
0
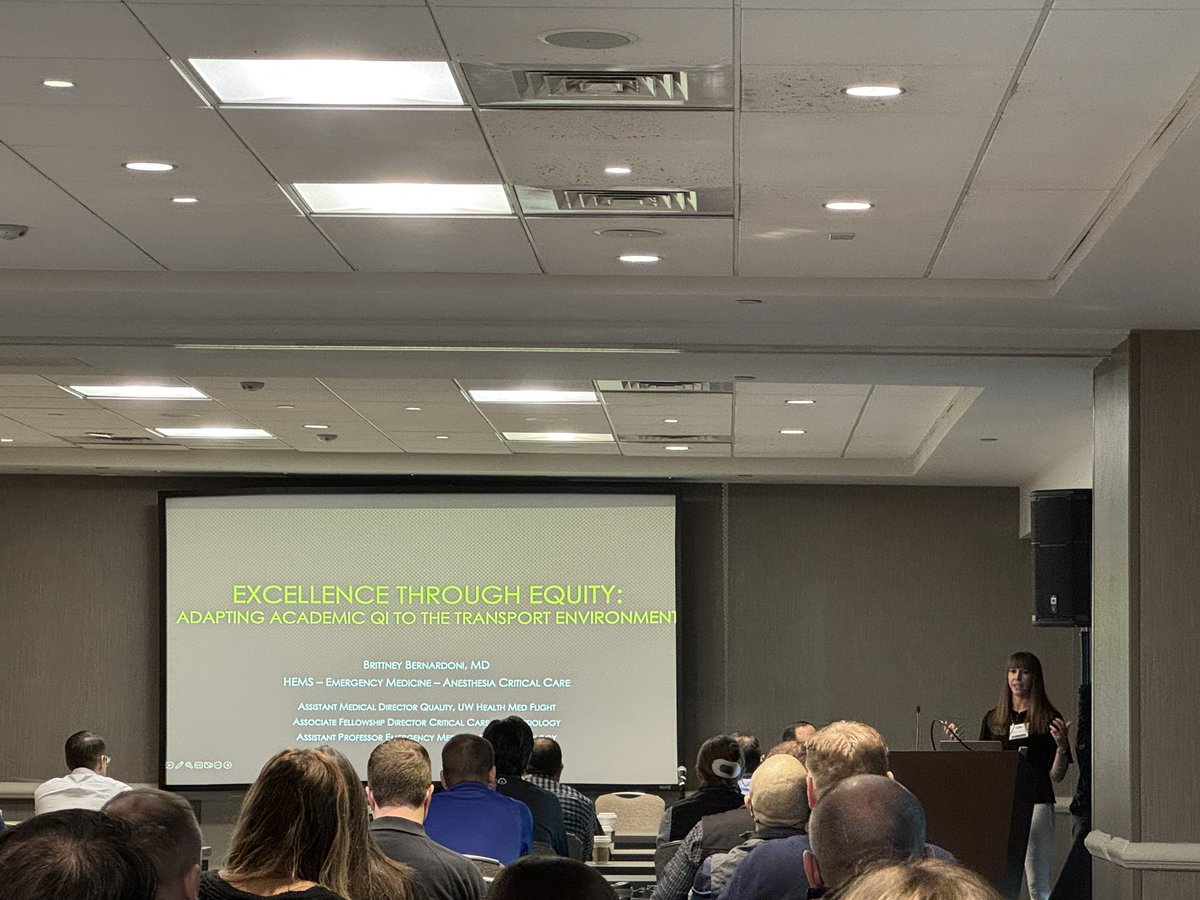
Another great talk from @BBernardoni_MD @AMPAdocs @UWMedFlight a masterclass on refractory hypoxia, utilizing delta pressure, pplat to help guide protective lung recruitment. Use of epoprostenol. Caution initiating proning & reverse I:E just prior to transport @NAEMSP @UWEmerMed
0
6
10
Outstanding overview of our case review & peer review process @UWMedFlight by @BBernardoni_MD @AMPAdocs presumption of positive intent, multidisciplinary team, initial review, crew feedback, peer review, coach the individual, improve system @NAEMSP @UWEmerMed @UCAirCareDoc
0
5
11
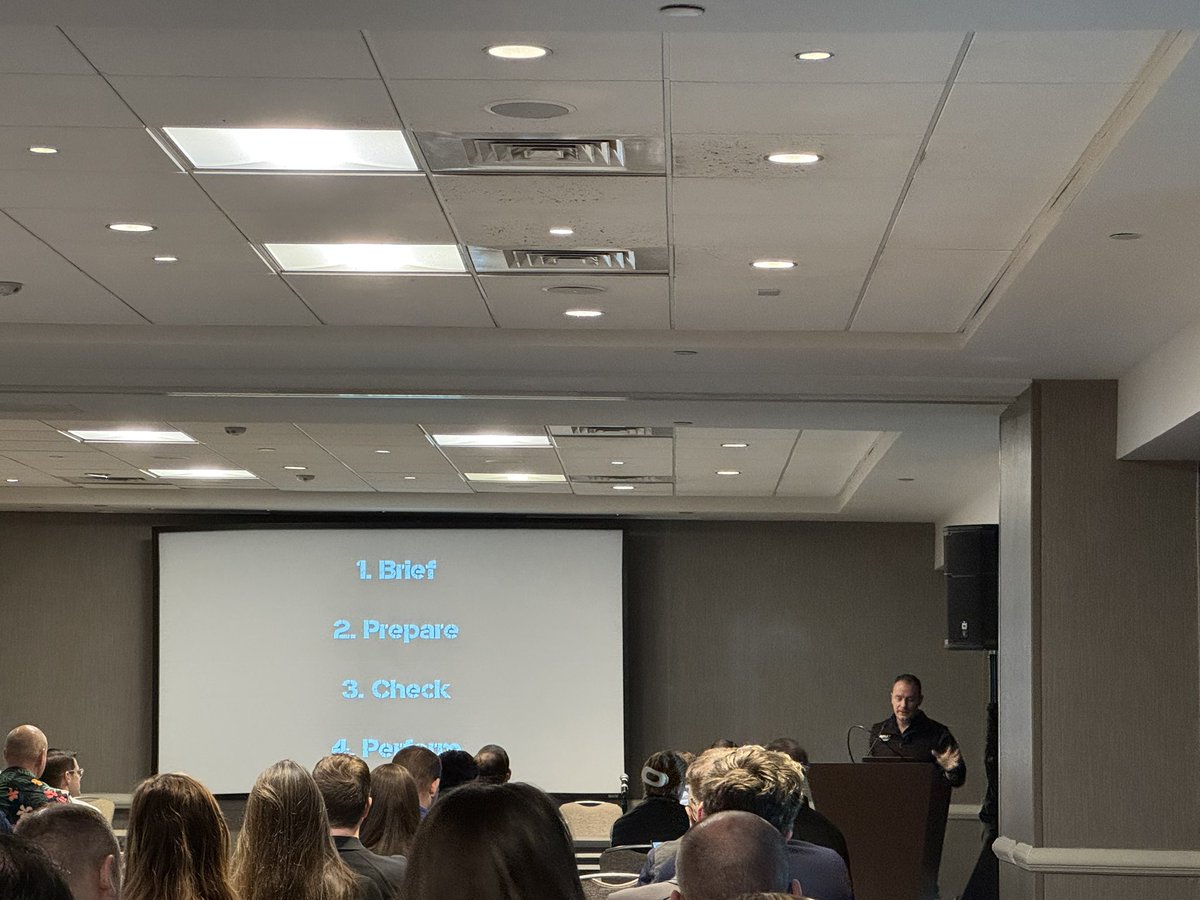
Excellent talk from @ResusPadawan on checklist design AMPS @NAEMSP. Brief, Prepare, Check, Perform. Design with end user in mind, not for last minute teaching or as loaded with extra “stuff”. @AMPAdocs @AirliftNW @UWashEM @UWEmerMed @UWMedFlight
0
3
11
Solid data that physicians presence within prehospital teams does matter to our patients. @AMPAdocs @NAEMSP @RCSEd @_retrieval @UWMedFlight @UWEmerMed @ACEPNow
0
7
22
One of our first year residents, Lera O’Sullivan, with EMS fellowship plans, getting hot loading training and a taste of the patient experience on one of her flight shifts with us. @UWMedFlight @MadtownEM @UWEmerMed @AMPAdocs @NAEMSP @mack99301
0
3
17
RT @UWHealth: After 30+ years transporting patients with @UWMedFlight, Dr. Mike Abernethy became a patient when diagnosed with cardiac dise…
0
7
0
RT @DrewCathers: Our last @UWMedFlight education and simulations of 2024! TBI, ischemic CVA, Obstetrical transport and airway skills review…
0
4
0
RT @JTraumAcuteSurg: Preoperative CT scans do not provide a “roadmap” for patients with abdominal gunshot wounds who undergo a laparotomy.…
0
32
0
@AliHusain82 @AMPAdocs @jasumback @LawnerBen @laertezz Yes this was the discussion, and even then only contemplated in the eminently dying trauma patient in the prehospital setting, where without obtaining an airway the patient would be moments from death. Even then resuscitation in parallel is essential.
0
2
4
As a new Emergency Medicine attending 10 years ago I was asked to write about my insights into what it's like to be an ER Doctor. I just randomly came across it and after all these years I'm amazed by how much this all still rings true in my heart today. So I wanted to share it with you guys. Here's what I wrote: MAKE THINGS HAPPEN, SAVE LIVES, ALLEVIATE SUFFERING My Emergency Department is a battlefield. Volumes are high and the pace is fast. To succeed as an Emergency Physician I must be an expert of efficiency. I also must be an expert of triage. I am constantly triaging and re-triaging as things evolve. The ED is highly unpredictable. My entire shift I am on guard and ready for any emergency to come flying through the doors at any moment. In the meantime I am either taking care of or seeking out other emergencies. My job is not to be expert in all of medicine. My job is to be jack of all trades and master of diagnosing and treating what can and will kill you. If I cannot provide the definitive care you need, my job does not end until I have gotten you there. The more I practice Emergency Medicine, the more I realize that what I do more than anything else is - make things happen. Cliff Reid (@cliffreid) delivered an excellent SMACC talk on making things happen in the resuscitation bay. (If you haven’t yet heard it I recommend you do). I’ve come to realize that this concept extends beyond the resus bay and pervades all aspects of my job. So what does it mean to make things happen? Making things happen means putting my visions of what needs to happen into motion and making them reality. In order to make things happen, I must first appreciate that my ED is equipped with an army of highly skilled staff that are the heart and soul of the department – and that without them I could make very little happen. Making things happen means identifying a sick patient and getting them quickly moved to a critical bed; it means getting my suspected head bleed patient expeditiously to the CT scanner with least possible delay; it means mobilizing help to intervene on my flash pulmonary edema patient in hypertensive crisis and getting her on CPAP & Nitro immediately to pull her out of the water and prevent intubation; it means convincing my adamant patient who is ready to walk out the door but is clearly not well enough to go home not to sign out against medical advice, but rather to stay in the hospital where he/she is safe and taken care of; making things happen means advocating for my patients and convincing my consultants to take them emergently to the cath lab or operating room at 3 AM when it otherwise would not have happened until morning. Making things happen means constantly thinking two steps ahead. Making things happen is an art. I have learned that to excel in Emergency Medicine I must master the art of making things happen. If my goal is to save lives, I must first recognize that a life needs to be saved – that is, I must be an expert at diagnosing life-threatening processes. The 75-year-old clutching his chest with tombstones on his ECG – that’s easy. The problem is that most of my patients are not truly sick. Some are here because they are afraid that they are sick, and just need reassurance. Some are here just for pain medications. Most of my patients are undifferentiated. Sickness is a spectrum. Truly sick patients often look sick, but often they do not. I must be expert at sifting through the crowd and identifying which patients are harboring a life-threatening diagnosis. This is not always an easy task, but it’s up to me to figure it out. It’s my job to figure out that the 45-year-old gentleman who looks comfortable sitting up in bed watching television and texting on his phone has a Type A Aortic Dissection. If I simply get two sets of cardiac enzymes, repeat an ECG and discharge him home since these are normal – there is a good chance he will die. It’s my job to figure out that the 60-year-old lady with chest pain who was transferred to me for “NSTEMI” actually has a huge saddle pulmonary embolus. It’s not enough to just admit her to the hospital floor only for her to sit up there, decompensate, and have a bad outcome. I have to do better than that. In the Emergency Department, there are landmines scattered everywhere. It’s my job to find the landmines. I can’t talk about saving lives without talking about Resuscitation. This is an entire topic in and of itself and I could write all day about it – but I won’t do that here. I will simply say that if I want to save lives, I must be an expert at Resuscitation. I believe that as an Emergency Physician, if I am not expert at Resuscitation – my purpose is lost and my mission is in vain. Resuscitation encapsulates those moments that matter most; the moments that often determine my patients’ fates, and define Emergency Medicine as a specialty. Resuscitation is the essence of Emergency Medicine. In the end, Emergency Medicine is all about the patients. While patients are under my care, I consider them family. When I walk into a room, I shake hands with each patient and all their friends and family members who have come to support them. I look my patients in the eyes. I listen to them. I try my best to put myself in their shoes and empathize with them. I know that communication is vital and I make sure we are on the same page, and that all of their questions have been answered. I make a point to ensure that they know to let me know if they need anything. If my patients are not comfortable, I am not comfortable. Some humble advice I have to offer for success in Emergency Medicine: 1. Never stop learning. There’s too much out there to know, and knowledge is the foundation for the care we provide. Your eyes won’t see what your mind doesn’t know. Never get complacent in your knowledge. 2. Trust your instincts. Gestalt is at the heart of what we do. Without it we are merely computers and robots. Gestalt trumps any clinical decision rule any day. Even if you don’t know exactly what’s wrong with your patient, but you have a feeling something bad is going on – trust it and pursue it. 3. Be decisive. I’ve seen too many times patients crash while “decisions were being made”. If you choose not to intervene that’s fine, but not intervening should never be the default decision, as a result of indecision. That is unacceptable. First do no harm, does not mean do nothing. Don’t fall victim to being more comfortable with the devil you know than the devil you don’t. Understand that sometimes not taking a risk can be extremely risky. 4. Learn to control your mind in stressful situations. Adrenalinization is normal. While it’s a natural reaction and will enhance your performance, too much will impair your thought process and technical skills. Learn to recognize when you’re becoming over-adrenalized, and learn whatever it is that works for you to be able to relax, stay calm, and temper your sympathetics. 5. Be cognizant of human factors. So much of what we do is psychological. Be aware of your susceptibility to cognitive bias. The key to conquering cognitive errors is to be aware of their existence. 6. Debrief after codes or tough cases and take time to reflect back after shifts. I do this routinely and I find it to be invaluable. Some of the greatest things I have picked up on have been via this process. 7. Learn Emergency Ultrasound.Believe me when I tell you that Emergency Ultrasound will transcend your practice. If you don’t learn EM ultrasound, at least learn the critical care stuff. If you don’t learn the critical care stuff, at least learn basic Echo – it has the greatest impact. 8. Follow up on your patients. I can’t express how much of my learning is through following up on my patients. If you don’t do it already – start! You will be amazed by how much you will learn. 9. Accept and embrace that some of your patients will have bad outcomes or die no matter what you do – but never, ever let this be an excuse to provide anything less than the best care you possibly can. 10. Be kind and compassionate. When it’s all said and done our patients may not remember details of their ED stay during what might very well have been the worst day of their lives – but they will remember how we made them feel.
2
1
17
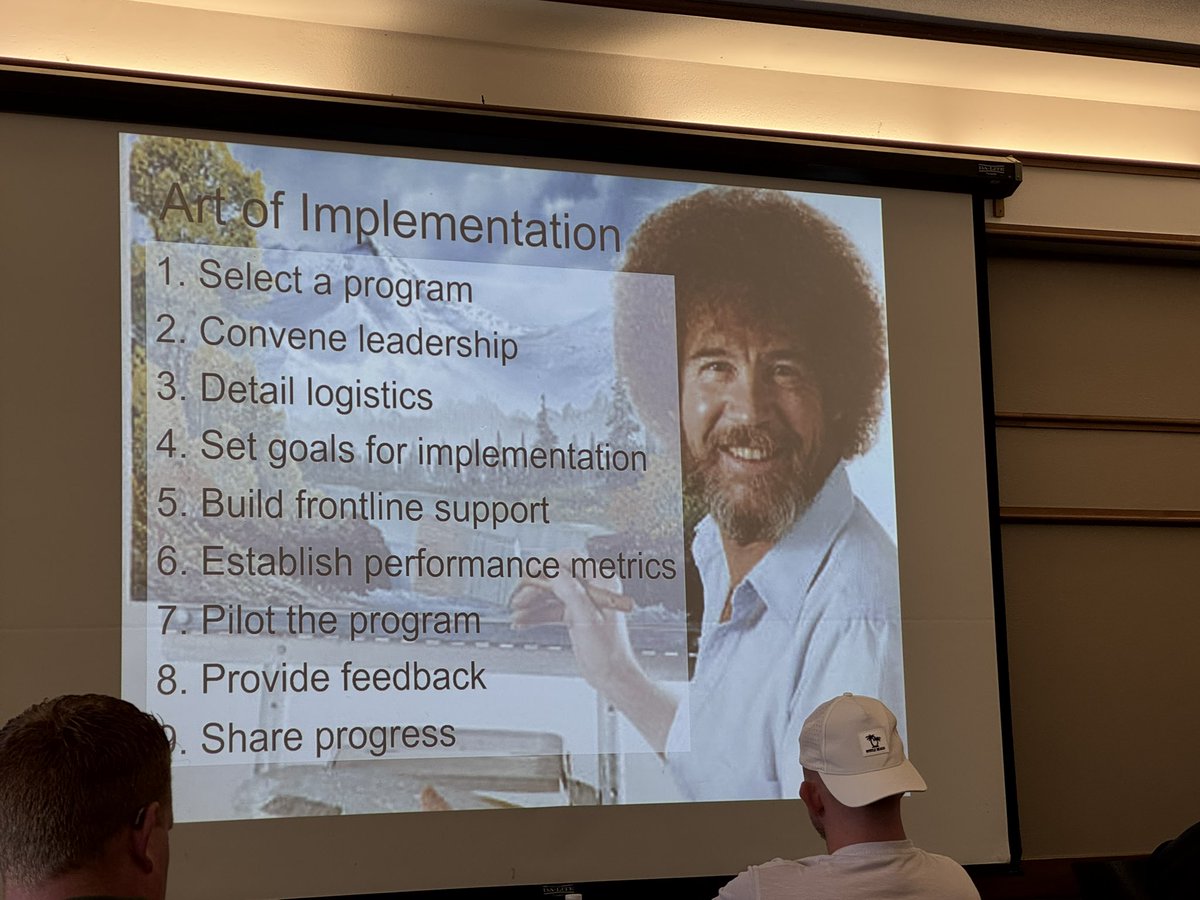
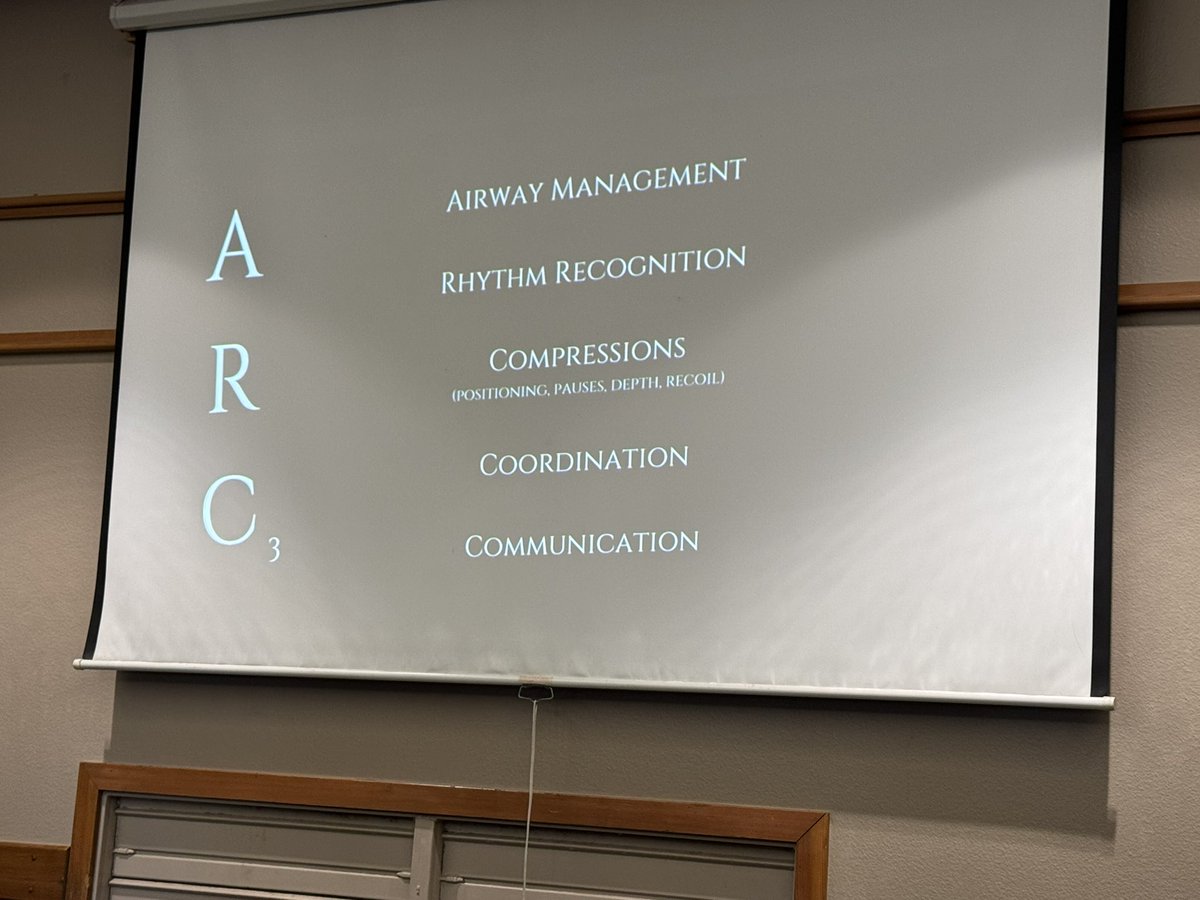
Great 2 days at @ResuscAcademy a lot of things to bring back to @UWEmerMed @UWMedFlight key is not just ideas but implementation, measure and improve with iterative changes. @AMPAdocs @NAEMSP @ACEPNow @_retrieval @MadtownEM
0
3
6
Absolutely brilliantly talk on debriefs from @bp_mcneilly, top down driven process to open the dialogue. What was expected, what occurred, difference, how do we improve? @AMPAdocs @NAEMSP @UWEmerMed @MadtownEM @UWMedFlight @_retrieval
0
1
9
Insightful overview of the outstanding work done by @AmbulanceVic from @expensivecare on their over two decades of being on a mission of excellence and highlighting the need for ongoing deliberate work and quest to improve. @AMPAdocs @NAEMSP @UWMedFlight @UWEmerMed @MadtownEM
0
2
14
@TotalResus @ResusPadawan @ResuscAcademy @AMPAdocs @NAEMSP @UWEmerMed @UWMedFlight @MadtownEM @_retrieval @EMRSscotland @DarrenBraude @UNMEMSA @ACEPNow While the evidence is not superb, norepinephrine was advocated as first line unless findings with POCUS support use of an inotrope
0
0
1