Erin Murphy
@TheVeinBoss
Followers
709
Following
315
Media
11
Statuses
117
Joined April 2022
A week of great friends and outstanding education. Fun at the meetings and out on the town! And yes, Kush Desai’s sign says Erin Murphy and I love it ;) @CXSymposium @kush_r_desai @GeorgeAdamsMD @KathleenGibson6
5
3
46
Another outstanding Cx 2022 session. Currently speaking Eric Secemsky, MD presenting an expert consensus on IVUS use for PAD interventions. #IVUS #Ericsecemskymd
0
0
36
In the past week I have had the opportunity to work with such great friends and colleagues! First stop - Miami to coordinate a Venous Summit with Peter Schneider sponsored by Philips. Thank you Philips for the opportunity! @PSchneiderMD @LessneVIR @KathleenGibson6 @PhilipsHealth
1
1
29
@farkomd @HCrespoSotoMD @lahinchman @UkVenous @KaremHarthMD @LessneVIR @RKTvascular @theveinlady @ReneLizola @HYY1084 These are the venograms pre & post endophlebectomy and then after additional stenting. Note the CFV disease prior to endophlebectomy. Grateful to have a talented colleague like Dr CrespoSoto to do these cases with.
3
4
29
The Charring Cross 2022 executive board at work. It was an honor to be involved and work with my highly esteemed colleagues. An excellent meeting. Look forward to the future. @CXSymposium @UkVenous @ManjGohel, Dr. Armando Mansilha
0
2
15
@VascularSVS @s_brathwaite @kush_r_desai @MinaMakaryMD @KaremHarthMD 2. If symptoms are primarily lower extremity or vulvar varicose veins, I generally will treat the presenting complaint with phlebectomy or sclerotherapy first and re-evaluate. If pelvic pain is the primary complaint, I obtain cross-sectional CTV imaging.
1
1
10
@AmputationSuck 1. IVUS is important for an accurate diagnosis. It reduces the risk for over treatment while improving outcomes by helping ensure that disease is appropriate for stenting, stent sizing is adequate, landing zones are correct, & inflow is adequate.
2
1
9
@VascularSVS @s_brathwaite @kush_r_desai @MinaMakaryMD @KaremHarthMD 1. I first evaluate the patient’s symptoms and perform a physical exam. I am interested in teasing out whether the patient’s symptoms are primary pelvic pain, labial varices, or lower extremity varicose veins that originate from a pelvic source.
1
1
9
@VascularSVS @s_brathwaite @kush_r_desai @KaremHarthMD @MinaMakaryMD Venous ulcer disease is secondary to high venous pressures. It is important to evaluate all underlying causes of venous HTN inclusive of deep venous disease, superficial venous disease and medically induced venous HTN. Further treatment is then dictated by the underlying cause.
4
0
9
@KaremHarthMD @farkomd @HCrespoSotoMD @lahinchman @UkVenous @LessneVIR @RKTvascular @theveinlady @ReneLizola @HYY1084 Thanks Karem. This patient had bulky CFV scar that did not respond to angioplasty & blocked the profunda. My criteria is a healthy profunda (and ideally femoral) just prior to the confluence to assure good inflow. Stenting is then performed into the patch from the IJ.
1
1
8
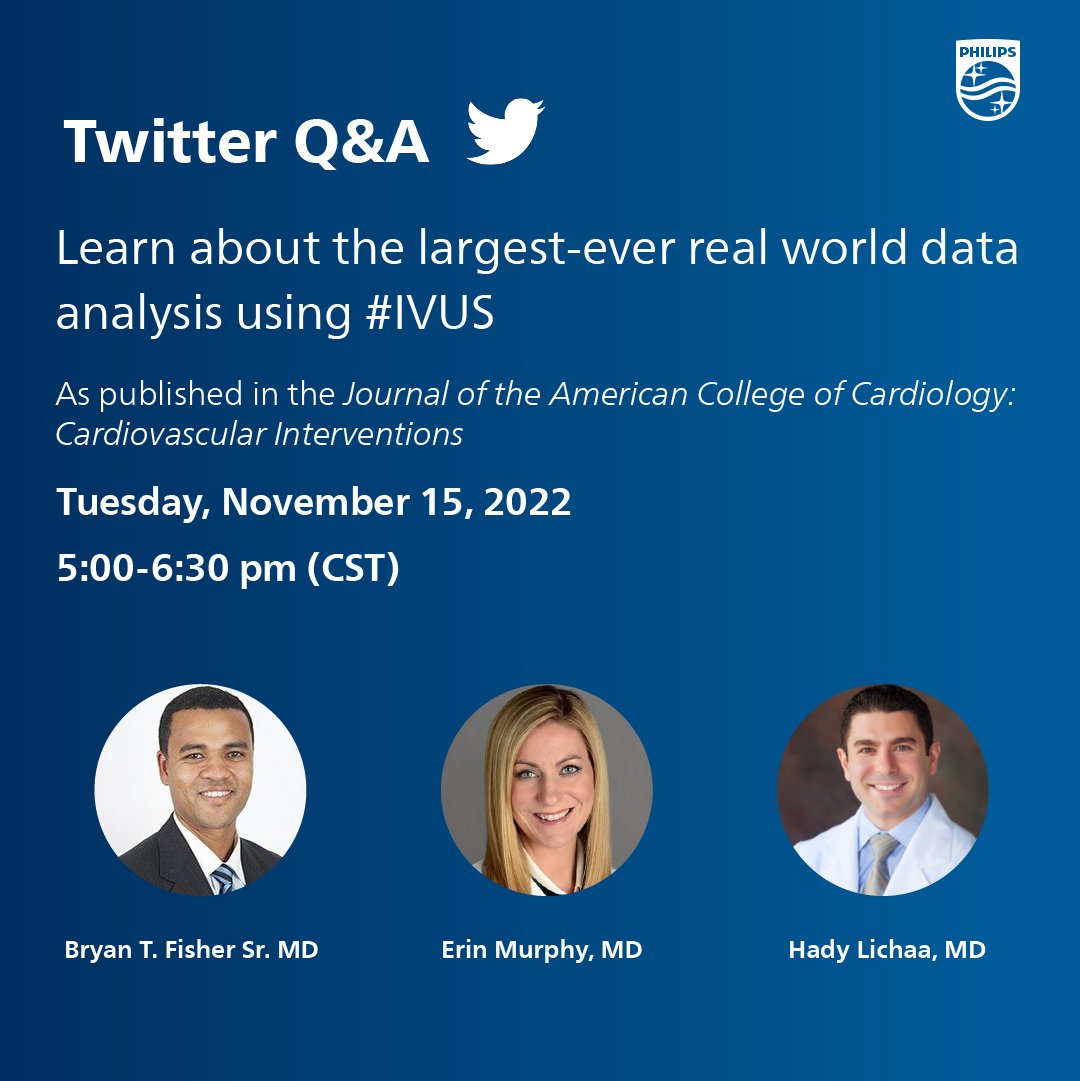
Our live Twitter Q&A from 5-6 pm CST on #IVUS will begin! Looking forward to chatting!.
On November 15th, vascular experts @AmputationSuck, @TheVeinBoss, and @HadyLichaaMD will be answering all your IVUS questions during a live Twitter Q&A. Submit your questions now using #IVUS.
0
0
7
@VascularSVS @s_brathwaite @kush_r_desai @KaremHarthMD @MinaMakaryMD My follow-up for deep venous interventions is US stent checks at 2 weeks, 3- 6- and 12- months then annually. For Patients with IVC stents, I generally obtain an additional CTV at the post-op 3-6 month point. While not routine in all practices, I perform US 2 days after RFAs.
1
0
8
@farkomd Thank you Frank :) We have sure come a long way in the past 18 years!! Hard to believe I have known you that long….
0
0
7
@HadyLichaaMD @AmputationSuck I anchor these stents well into the EIV to assure adequate stent fixation. This prevents both (1) landing of shorter stents in the dilated distal CIV and (2) Landing shorter stents in the pelvic curve with resultant frequent complications.
0
0
7
@VascularSVS @s_brathwaite @kush_r_desai @KaremHarthMD @MinaMakaryMD I evaluate superficial disease with duplex US and deep disease with US of the iliac veins and cross-sectional imaging, typically CTV.
1
0
7
@KaremHarthMD @farkomd @HCrespoSotoMD @lahinchman @UkVenous @LessneVIR @RKTvascular @theveinlady @ReneLizola @HYY1084 Luckily, I have great colleagues to partner with on these complex cases. Hector is a rockstar.
1
2
7
@AmputationSuck 1. Deep venous related leg ulcers should be managed comprehensively. This includes evaluation and management of superficial venous disease and deep venous obstruction. Perforator disease may have a role in some patients.
1
2
7
@LessneVIR @SIRspecialists @VascularSVS @kush_r_desai @lahinchman @KaremHarthMD @kmadass @Watts_IR @AmputationSuck @keithppereira @SDhandMD @ABrandisMD @t_intheleadcoat It was my privilege Mark! Great day.
0
0
6
@t_intheleadcoat @HCrespoSotoMD @farkomd @lahinchman @UkVenous @KaremHarthMD @LessneVIR @RKTvascular @theveinlady @ReneLizola @HYY1084 Initial DVT was managed with AC only. Recurred after stopping AC & was treated with indefinite AC. I attempted an endo approach 1st but the cfv disease was very bulky, unresponsive to venoplasty & blocked profunda flow. Inflow prior to the fem/profunda confluence was healthy.
1
0
6
@VascularMD @farkomd @jmills1955 Darren… agree that @jmills1955 is charged with promoting the specialty of vascular surgery. Also believe he set us back dramatically in that end. He should instead be suspending the svs membership of the surgeons who contributed to that NYT article for unprofessional behavior.
1
1
7
@HadyLichaaMD @AmputationSuck In diffuse PTS, the more difficult aspect is finding a landing zone clear of disease and ensuring no disease is left between the end of the stent and the profunda-femoral confluence.
1
2
5
@jcgeorgemd @SCAI @EricSecemskyMD @sahilparikhmd My honor to speak at SCAI and share the stage with such esteemed colleagues! Great to see you all!.
0
0
5
@drochohan @ImagingDoctor @LessneVIR @kush_r_desai @CHICKVIR @IR_Doctor @bonesz @VenousForum Fracture of wallstents through septum - left was previously collapsed by right but I dilated them and fractured them. Next post is end result. Converted double barrel to one large stent then extended down iliacs.
0
0
5
@VascularSVS @s_brathwaite @kush_r_desai @KaremHarthMD @MinaMakaryMD In my practice, I find RFA & sclerotherapy produce excellent results in the vast majority of patients with little need for deviation. Providers with alternative technology preferences also have great results. Decisions depend on device cost, comfort, safety, & success profiles.
1
0
5
@kmadass @AmputationSuck 2. However, in most cases, recurrent thrombosis is more often associated with profunda inflow (overlooked with PMT devices without lysis), failure to treat the outflow obstruction adequately, as well as technical errors with stenting.
1
0
5
@HadyLichaaMD @AmputationSuck In these cases sizing is actually easier. I size to normal vein sizes which roughly are CFV: 12, EIV: 14, CIV 16. So generally I will use 14 stents distally and 16 stents cranially.
0
1
5
@HYY1084 @HCrespoSotoMD @farkomd I thought of you two and your Atrium socks when I was given these to wear in clinic this morning.
1
0
4
@kush_r_desai @VascularSVS @s_brathwaite @KaremHarthMD @MinaMakaryMD A few less IVC filters when we are done with them :).
0
0
4
@farkomd @KaremHarthMD @HCrespoSotoMD @lahinchman @UkVenous @LessneVIR @RKTvascular @theveinlady @ReneLizola @HYY1084 Yes of course! Who trained him again? ;).
2
0
4
@kush_r_desai @VascularSVS @s_brathwaite @MinaMakaryMD @KaremHarthMD This is such an important perspective. This can make early ventures into this space discouraging if you do not have a team approach.
0
0
4
@kmadass @AmputationSuck 1. It is certainly not wrong to use tibial vein access for lysis so I am not actively discouraging this approach even in the first attempt if that is an interventional preference.
0
0
4
@s_brathwaite @limbsalvagedr @VascularSVS @kush_r_desai @KaremHarthMD @MinaMakaryMD I treat early with ulcer bed sclerotherapy, often at time of venous closure. I do wait 6 weeks before considering perforator treatment.
1
0
4
@LessneVIR Gallons per year?? Yikes… Im way behind. But I am catching on to this twitter thing.
2
0
4
@AmputationSuck In the awake patient, I use both Valsalva and breath-hold maneuvers while using IVUS to image the suspected compression. Valsalva alone can cause compression via contraction of abdominal muscles (will resolve with breath hold). Under anesthesia, Valsalva is sufficient.
0
2
4
@DejahJudelson @VascularSVS @s_brathwaite @kush_r_desai @MinaMakaryMD @KaremHarthMD I find that my decision between MRV and CTV depends on your comfort level and the quality of those imaging modalities at your institution. I find CTV more universally applicable but MRV works great if your radiology division does a great job with these.
1
0
4
@UkVenous @MDTVascular @myAVLS @TheVEINSatVIVA Back at you Stephen. Always an honor to work with you.
0
0
4
@SriniTummala @LessneVIR @SIRspecialists @VascularSVS @kush_r_desai @lahinchman @KaremHarthMD @kmadass @Watts_IR @AmputationSuck @keithppereira @SDhandMD @ABrandisMD @t_intheleadcoat Mark- That is 2 men that commented on your looks… I must be losing my touch or… you are THAT impressive! Hmmm… both?.
2
0
4
@jmills1955 @VascularMD @farkomd Likewise, if there are professional concerns, the clear pathway to address them exists. This pathway should not be the New York Times. As a society maybe we could address that as inappropriate?.
0
0
4
@jmills1955 @VascularMD @farkomd From the policies you referenced… Likely not professional or smart for physicians to discuss colleagues and medical professional issues with the NYT. Is that the environment we want to practice medicine in? Or is this an issue for professional conversations and medical boards?
3
0
3
@kush_r_desai @VascularSVS @s_brathwaite @KaremHarthMD @MinaMakaryMD With superficial veins, you need to make sure you use tumescent to keep the vein 1cm from the skin or perform phlebectomy if outside the fascia.
0
0
3
@AmputationSuck 2. Overall, IVUS improves patient selection and reduces complications to improve outcomes.
0
0
3
@kush_r_desai @VascularSVS @s_brathwaite @KaremHarthMD @MinaMakaryMD As long as there is a short straight segment of vein cranially you can utilize RFA followed by sclero once the cranial portion of the main vein is closed.
0
0
3
@farkomd @AmputationSuck Yeah… um… Frank? Maybe share exactly what happened to that bird that got in your house? I think I heard this story… I seem to recall key words of salt gun? Bookshelf? Someone will find its body someday?.
2
1
3
@GrahamSlessor @LessneVIR @farkomd @VascularSVS @SIRspecialists Maybe his lead helped me to channel his skill… and this way he also gets partial credit for my case without showing up ;).
1
1
3
@UkVenous @academicaorta @farkomd @HCrespoSotoMD @lahinchman @KaremHarthMD @LessneVIR @RKTvascular @theveinlady @ReneLizola @HYY1084 Agree selection is key. This patient had no great endo alternatives as the cfv disease was unresponsive to venoplasty & blocked profunda inflow. Fortunately the profunda & femoral v were healthy before the confluence. The residual iliac occlusive disease was treated with stenting.
0
0
3
@drochohan @AmputationSuck @kmadass Since we do not have great interventional options for fem-pop DVT later on, I generally treat these with lovenox and re-evaluate improvement @ 2 weeks. I reserve intervention for highly functional patients who will not tolerate even mild PTS and who are still symptomatic at 2 wks.
0
0
3
@docmrjaff @bsc_pi @bsc_vascular @sahilparikhmd Outstanding meeting! Proud to collaborate with Boston Scientific and an amazing group of physician leaders. Well done.
0
0
3
@drochohan @ImagingDoctor @LessneVIR @kush_r_desai @CHICKVIR @IR_Doctor @bonesz @VenousForum Caval wallstent and arterial (smart) stents? The Ivus would dictate treatment. Smart stents can be broken and restented larger if not occluded. Also If collapsed in IVC can possibly fracture the septum and convert to a large caval stebt then extend down iliacs as needed.
0
0
3
@AmputationSuck 2. Medical management of disease contributing to venous HTN is essential (Obesity, heart failure, etc). Compression, wound care and lymphatic care are also important.
0
1
3
@docmrjaff @YolandaCDBryce @MaureenKohi @MdTabori @kush_r_desai @drksterling Excellent topics and top notch physicians! Thank you Boston Scientific for supporting education and field advances!.
0
0
3
@TobyRichardsUWA @farkomd @HCrespoSotoMD @lahinchman @UkVenous @KaremHarthMD @LessneVIR @RKTvascular @theveinlady @ReneLizola @HYY1084 Agreed. In this case the disease was involving the origin of the profunda inflow. A CFV stent would have left the profunda flow severely compromised.
0
0
3
@dr_ashishg @PSchneiderMD @LessneVIR @KathleenGibson6 @PhilipsHealth Thank you. It was so great to meet you as well.
0
0
2
@JillSommerset @LessneVIR @farkomd @HCrespoSotoMD I plan to fly in and out for a talk. Not much focus on venous. But I will let you know as soon as I make travel plans- We WILL make it happen :).
1
0
2
@HadyLichaaMD With the current stents on the market, the risk for stent fracture is very rare (or a never yet event for some of them). To minimize pain and risk, make sure to size accurately (generally 14 mm stents across the ligament) and avoid overlapping stents across this location.
0
0
2
@AmputationSuck @kmadass 1. Inflow is very important to the eventual outcome for patients as is the amount of thrombus removal. In general, I access the popliteal vein as complete thrombus removal above this followed by relief of associated obstruction with stenting allows the tibial clot to resolve.
1
0
2
@AmputationSuck @kmadass 2. The SSV is also a helpful access to clear popliteal clot as long as the SSV in fact communicates with the popliteal vein.
0
0
2
@HCrespoSotoMD @LessneVIR Yes! Large pelvic varices for sure! So much for menopause fixes pelvic congestion- not always the case.
0
0
2
@HadyLichaaMD @AmputationSuck I avoid stenting into the profunda or femoral vein but you can venoplasty these vessels.
1
0
2
@HCrespoSotoMD @HYY1084 @farkomd I just know that is referring to the scrubs and not how I am wearing them 😜 We cannot all be as cool as you guys and your socks :).
0
0
2
@KaremHarthMD @farkomd @HCrespoSotoMD @lahinchman @UkVenous @LessneVIR @RKTvascular @theveinlady @ReneLizola @HYY1084 Absolutely!.
0
0
2
@DrLizGenovese @CXSymposium @kush_r_desai @GeorgeAdamsMD @KathleenGibson6 You would have fit in perfectly- look forward to seeing you again soon :).
0
0
2
@farkomd @radcliffeVASCU @UkVenous @vascularIR @DoctorGreg13 @limbsalvagedr @gkorosoglou @b_modarai THIS! I came here to say just this!.
0
0
2
@PipeCabreraV @CXSymposium @kush_r_desai @GeorgeAdamsMD @KathleenGibson6 Absolutely. Erinmurphy79@gmail.com.
1
0
1
@JayMathewsMD @UkVenous @theveinlady Owes? Well I am not so sure about that… But I do share well with friends :).
1
0
1
@KutsenkoMD @farkomd @VascularSVS Yes interesting timing… .SvS- “Don’t worry we will train you”.Recent NYT cardiologist “I was teaching you at the recent 2023 VAM meeting”.
0
0
1
@EstherSHKimMD @Angiologist @herbaronowMD @RKolluriMD @evratchford @SVM_tweets Esther! I look forward to meeting you soon. I am also at Sanger :).
0
0
1
@JamesHBlackMD @farkomd Have you reviewed these cases? Has SVS? Neither has the radiology & cardiology community. Condemning a physician publically in response to a sensationalized news story that acts like there is a public conspiracy committed by physicians and industry is arrogant, sloppy & dangerous.
0
0
2
@JillSommerset @LessneVIR @farkomd @HCrespoSotoMD Jill! Will you be at SCAI or NCVH? Maybe we can finally meet up?.
1
0
1
@lahinchman @JohnMoynes Haha… I just practiced that out loud a few times… Makes me sound more Irish! Making Murphy’s proud :).
0
0
1
@drmcumming @AmputationSuck There is certainly some of this which is not encouraged. But there is also the many decades of undervaluing of the significance of venous disease by vascular providers with the resultant under treatment of patients. There is some continued dismissal still evident here.
0
0
1
@farkomd @jmills1955 @DHidlayVIR @shamitsdesai @chrisharnain @VascularSVS @ashkan_1670 “Some”…. Hard to hide bigotry even when trying to hide bigotry.
0
0
1
@GrahamSlessor @LessneVIR @farkomd @VascularSVS @SIRspecialists Who? Another doctor … that’s who ;).
0
0
1