Nicholas Chrimes
@NicholasChrimes
Followers
8K
Following
6K
Media
573
Statuses
7K
Gone to Bluesky. Link to profile below.
Sydney, Australia
Joined March 2009
No one should be allowed to use the phrase “living with COVID” without defining what that means in terms of acceptable rates of hospital admission & death. #COVID19.
28
68
300
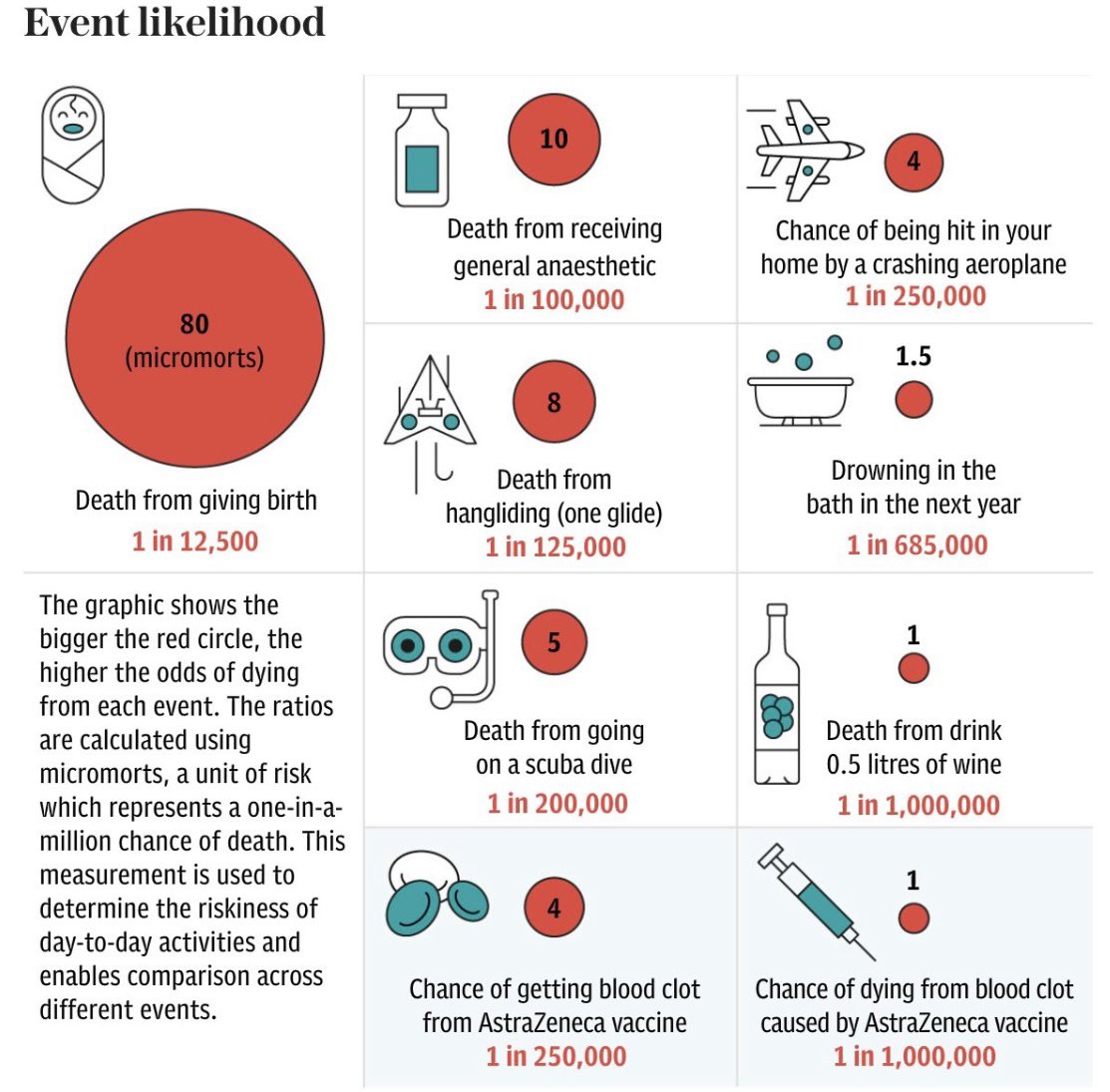
You’re 4 times more likely to be hit in your home by a crashing plane than to die from a blood clot from the @AstraZeneca vaccine. Graphic from London Telegraph.
16
190
311
18-39yr olds in Victoria who are not eligible under the current phase of rollout are now able to call and book an @AstraZeneca appointment through the National #COVID19 vaccine helpline! Much simpler than booking online & avoids the issue of GP’s declining AZ this group.
21
113
296
Aerosol boxes: longer times to intubation, lower 1st pass success & damage to PPE. Who'd have thought?. New study by @SpontVentGA @precordialthump @drdavidbrewster & Kent Lavery in @Anaes_Journal.
14
110
215
You seem to be ignoring: . ICU staffing requirements.Length of COVID ICU stay.Demands of care for COVID pts.Limited ICU reserves wout COVID.Exponential rise in COVID cases. Staggeringly incorrect.
Overwhelmed? The nation has over 2200 ventilators for immediate use and only 475 in use with only 33 of those used for COVID patients. Challenging?Yes. Tough on the frontline in Sydney? unquestionably. Overwhelmed? No. #factsmatter #auspol #COVID19nsw.
8
19
131
Stop using a self-inflating BVM. No feel for compliance, no ability to distinguish mask leak from obstruction if CO2 absent & diminishing FiO2 with increased MV. Use a flow-inflating bag like a Mapleson. It’s not harder, it’s just honest. If you have a leak the bag goes flat.
📢 Bag mask ventilation is the most underrated skills in emergency and critical care medicine!. Everyone thinks they are great at it, but very few are. Let's dive into the intricacies of Bag-Mask Ventilation (BMV) and shed light on some common problems associated with this
16
16
121
Could priorities & understanding of needs be more wrong?. Elective surgery will deplete consumables, block beds, increase transmission and prevent staff PPE training. All non-urgent surgery needs to stop immediately. #COVID19au .
6
46
109
Having had to cancel my 3rd ski trip due to Vic lockdowns I have just one thing to say to @DanielAndrewsMP…. Thankyou. Thankyou to you, Jeroen Weimar & @VictorianCHO for consistently putting the welfare of Victorians above what is easy or politically expedient.
10
10
90
Oxygen via Hudson mask can be placed OVER a surgical mask in #COVID19 patients without compromising FiO2. 🔐 Free in @Anaes_Journal .
1
70
93
Hypoxic bradycardia: does giving atropine treat the patient or the anaesthetist?. @AndyHiggsGAA, @nolittley & I give our thoughts on the matter in @Anaes_Journal. 🔓 🔑 .
10
46
79
Very proud of my 19yr old son @chriimes & his girlfriend for having their 1st dose of AZ #CovidVaccine today. A sensible decision to keep themselves & the community safe. The safest vaccine is the one you can get.
4
13
77
Rethinking TT size selection in anaesthesia. “Instead of opting for ‘the largest tube that the larynx will comfortably accommodate, we perhaps should consider using the smallest tube which permits the safe conduct of anaesthesia”. In @Anaes_Journal .
6
39
79
Wearing N95 masks in the absence of exposure to aerosols, to lower #COVID19 infection rates in HCWs is like wearing condoms even when you're not having sex, to lower the incidence of unplanned pregnancies.
30
22
80
I very rarely *need* a videolaryngoscope to get the tube in but I *benefit* from using it every day: improved teamwork, improved tube placement, less attempts, less trauma, less stress response (HAVL), etc. My team & I can just see better! Why would you want to see worse?.
🔓Human factors and teaching benefits of VL are based on evidence. ". we may not ‘need’ to use VL for every tracheal intubation, but we believe that there are significant benefits for the patient, ourselves and the whole team if we do.". 🔗
5
24
77
Just heard that there was an MCQ on the @VortexApproach in the recent @ANZCA fellowship exam. I have to say I’m pretty chuffed about that!
5
14
70
Why?.
🔓Remifentanil for tracheal intubation without neuromuscular blocking drugs in adult patients: a systematic review and meta-analysis. This great new paper is #OpenAccess and #FreeForever!. 🔗
21
17
71
To prevent 'hang up' when trying to pass an ETT into the trachea rotate anticlockwise above the cords & clockwise below the cords to facilitate the bevel clearing potential point of impact of the ETT. (@airwaycam may have come up with 'left & larynx, right at rings' before me)
4
45
69
For anyone not already aware of it “Airway Management in Emergencies: The Infinity Edition” by George Kovacs & @jadamlaw is an extraordinary resource. A free virtual textbook. A living document continually updated to reflect current best practice.
2
41
63
The videos from yesterday’s #WAMMHF session at #WAMMsterdam can be accessed at Many thanks to all who donated time & resources to making these incl @gerri59090195 @DrGivasHit @Krstin984 @SydneyCSSC @MonashAnaes @Simpact @WAMM_2019
6
36
67
There’s no valid reason to EVER use desflurane. No clinically significant benefits. Any theoretical benefits can be achieved better w propofol anyway. Environmentally catastrophic. Get rid of it. (if this wasn’t already obvious to you, here’s one more study).
🔐Does desflurane reduce the risk of postoperative respiratory complications when compared with sevoflurane?. This new cohort study from @lianazucco, @levy_ndv, @SarahNabel1 and @rsatyak suggests not, which may support decisions about its use. 🔗
7
25
59
Without question, the best video on hyperangulated videolaryngoscopy I've ever seen from @kovacsgj. Until you're familiar with all these points don't use HA-VL outside of a skill acquisition scenario - esp not on a COVID-19 patient.
1
30
61
Everyone who intubates should read this letter by @JPenketh39 @Fionafionakel & @doctimcook. Concise, well reasoned arguments regarding why & how we should use VL routinely where resources allow.
4
30
57
Of course it can. It demonstrates a complete lack of understanding of physiology. Sympatholysis in a hypovolaemic patient whose sympathetic response is the only thing keeping them alive is an assassination, not an induction.
Can ‘cardiac anaesthetic induction’ - high-dose opioids with a ⬇️ dose of induction drug - be implicated in maternal cardiac arrest in haemorrhaging patients?. Should we do a 'trauma induction' with eg ketamine instead?. 🔗
5
7
57
@willtube4food In my experience pts get justifiably upset if you expose them to a painful stimulus (they often are painful) wout warning. I ask them if they want be warned (most do), then use mitigating language (pinch vs pain) but not warning them at all is not a good approach in my opinion.
2
0
55
What’s the story @BJAJournals? Your content is generated for free & your reviewers work for free, you charge for access to most articles & sell advertising on top. If my college can’t afford your subscription, I won’t be submitting/reviewing any BJA articles.
@DrGetafix The 2022 cost to maintain the BJA subscription is an increase of over 1500% on our existing subscription & would use up more than 80% of the library’s entire annual budget. It would seriously impact our ability to continue offering a diverse & comprehensive collection.
2
12
56
@hoontangclan @ANZCA @hypoxicchicken @MonashAnaes @bigsaratoga @purplekimbo72 Free files to 3D print @VortexApproach neck rescue trainers (including separate neck/chin piece) are available for download at thanks to @edexam. #ASM21MEL
1
24
53
I’ve now been exclusively intubating using a videolaryngoscope (the technology) for about 6 months now but I rarely utilise videolaryngoscopy (the technique). #UniversalVL doesn’t mean sacrificing DL skills, it provides a video-capable device for #1stAttemptRescue when DL inadeq.
10
16
55
"The 'aerosol box' should not currently be used for intubation in most settings & is poorly suited to the management of critically ill patients. Further testing of the safety and effectiveness of the device is required". From @gaseousXchange in @LITFLblog.
5
24
55
“Finally, when the patient coughed, use of the aerosol box resulted in a marked increase in airborne particle exposure compared with other devices or no device use” 😂. Surprise 🥳🙄 from @Anaes_Journal .
7
33
52
@DrPieterPeach @michael_riordan 100%. To the extent that I’ve left work, driven home and been standing in my kitchen with it still on, until a member of my family has said “You know you’re wearing a mask right?” . (there would be a couple of N95 models that are significant exceptions to this).
1
1
48
.@DanielAndrewsMP deserves praise for the way he's handled the #COVID19Vic crisis. He's made tough (& not necessarily popular) decisions in the best interests of the community & taken responsibility for any errors made. It's rare to see leaders with such integrity these days.
1
6
48
I’m using 6,0 tracheal tubes for everyone these days unless there’s a specific reason to go larger (e.g. ICU postop).
🔐Sore throat after tracheal intubation can impair recovery. This new RCT finds that sore throat and hoarse voice 1 and 24 h after surgery were less frequent and less severe after intubation with smaller tubes. Ventilatory mechanics were unaffected. 🔗
6
11
50
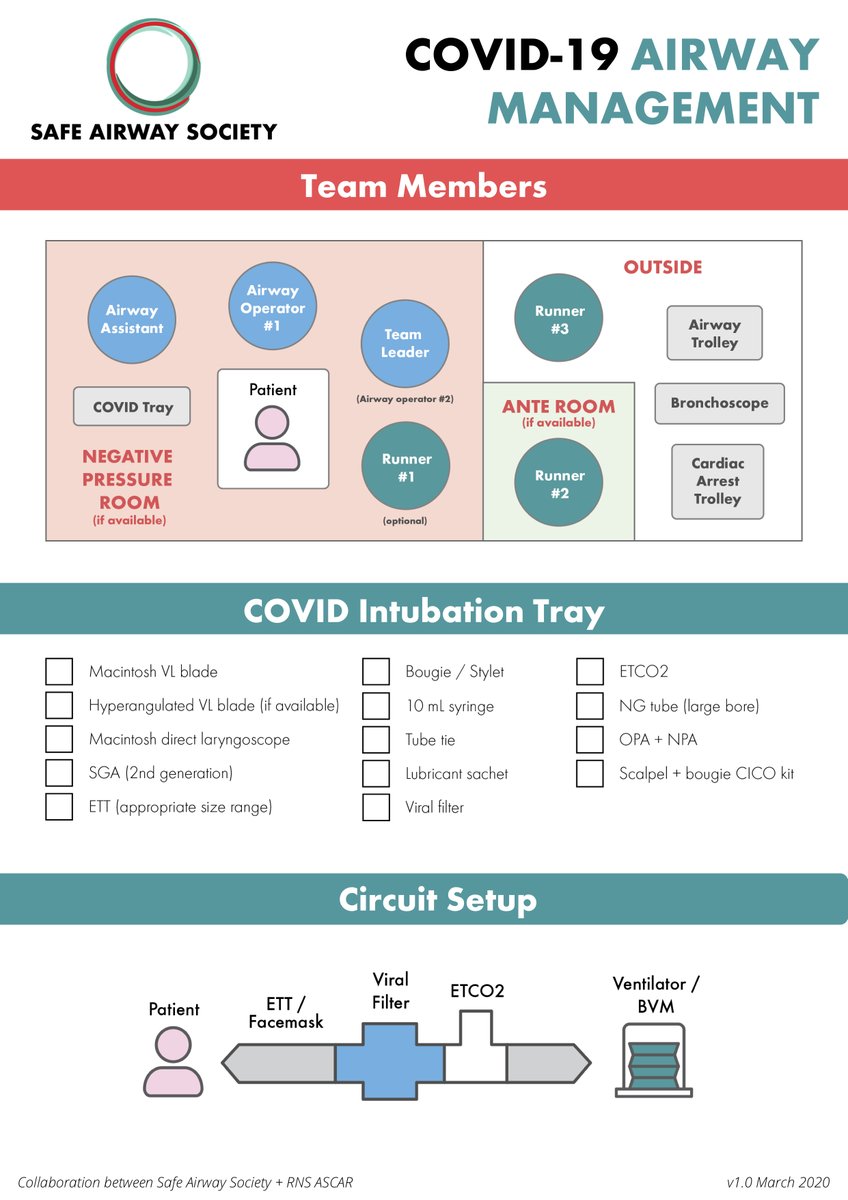
The @SafeAirway statement on airway management in the COVID-19 patient group in @theMJA has been endorsed by @anzics @CICMANZ @ASA_Australia @TheNZSA @acemonline @nzats @WAAGBali @ACPANurses. Outstanding work @drdavidbrewster @jgatward @precordialthump @DrGivasHit @cjgroombridge.
Consensus statement: @SafeAirway Society principles of #airwaymanagement and #intubation specific to #COVIDー19 adult patient group. Out now as pre-print version on @theMJA website to help front-line clinicians. Get training!
2
22
48
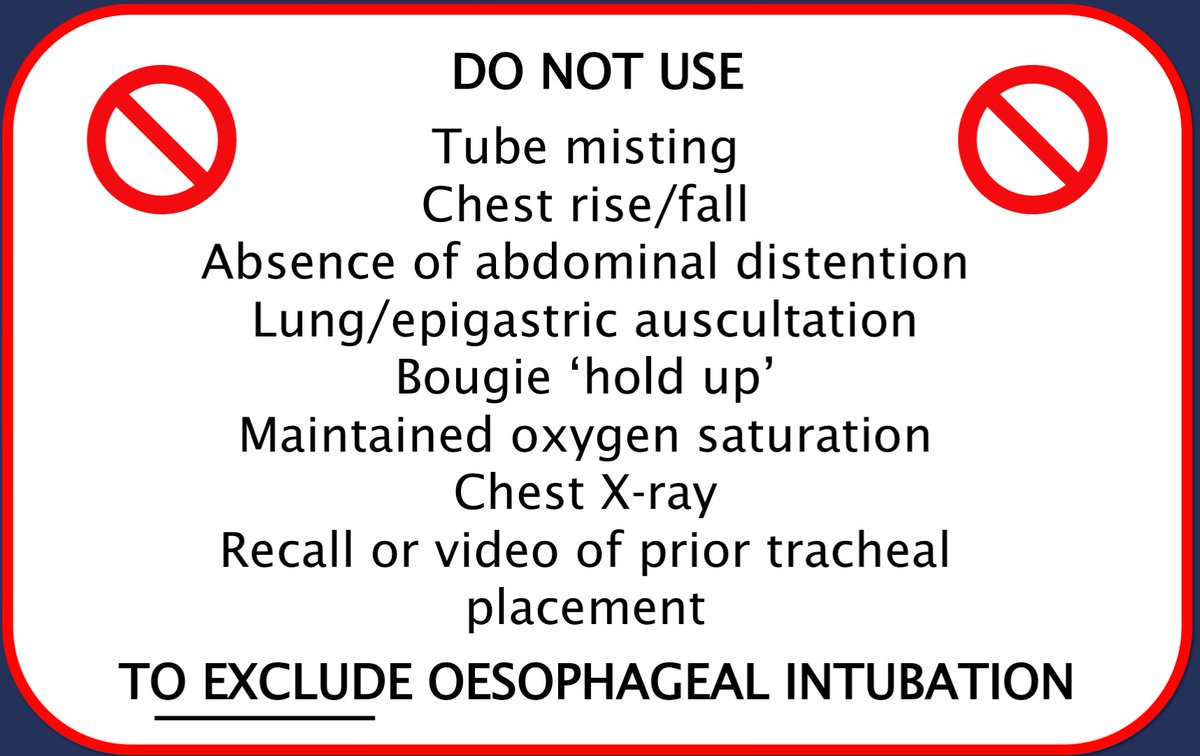
This editorial in @Anaes_Journal makes the absurd & dangerous proposal that ABGs be used to exclude oesophageal intubation in cardiac arrest patients receiving CPR. There are 3 BIG problems with this.
10
23
45
@VirtueOfNothing @AirwayMxAcademy @jducanto @NaveenEipe @airwayGladiator Managing tracheal tube hold up.
2
24
43
Is there any appetite for a @VortexApproach livestream? . Would be very simple: no guests, just me giving a 10 min presentation on an aspect of the Vortex followed by audience questions. If interested what topics would you like covered?
6
12
46
This review presents the data supporting what unexpectedly proved to be the most controversial recommendation in the ‘Consensus guidelines for preventing unrecognised oesophageal intubation’. Free full text in @Anaes_Journal 🔑🔓
Clinical tests for confirming tracheal intubation or excluding oesophageal intubation: a diagnostic test accuracy systematic review and meta-analysis. From @VirtueOfNothing @jadamlaw @NicholasChrimes @AndyHiggsGAA @doctimcook . Free🔑🔓in @Anaes_Journal.
3
32
42
By far the best video I've ever seen on HA-VL, from @kovacsgj. HA-VL is a core skill. Every aw operator with access to HA-VL should be familiar with this content. If you can "see the cords but can't deliver the tube" the problem is YOU not the device.
0
18
41
If ECMO team is ready at bedside, can ECMO be used as an alternative to #NeckRescue in a can’t intubate, can’t oxygenate situation?. Orlando Hung: No. Much too slow. Cannulas must already be in & pump primed to use ECMO for the anticipated difficult airway.
8
8
39
If you take issue with this statement, raise your concerns directly with @doctimcook @VirtueOfNothing & @ProfEllenO during this interactive livestream discussion on the essential nature of capnography.
2 days until our free, interactive panel discussion on capnography & preventing unrecognised oesophageal intubation. Register to receive a reminder email with the livestream link & an attendance certificate.
3
16
37
@jmpeyton @AirwayMxAcademy @DrRaniChahal @BobTeskey @doctimcook This can be a double edged sword. If the whole room wrongly *believes* they saw the tube go through the cords it can create a greater barrier to removal despite absence of ETCO2. Beware ‘glottic impersonation’.
5
12
38
The most impactful 5 mins of airway training in my career was with @gaspasser, teaching me his technique for #HAVL. Check out Richard’s virtual HAVL workshop on @AirwavesLive from earlier this year.
5
17
38
@DrEricLevi @LarynxUK Given an EMR brings not only the potential for benefit but also harm to patients, why isn’t it subjected to the same testing as a new drug or device before being introduced clinically? To my knowledge there’s no evidence they improve pt care and they certainly create new risks.
3
6
37
@LeahHoustonMD @CriticalCareNow @VirtueOfNothing @jducanto @AirwayMxAcademy @emcrit @RCoANews It doesn't sound like that or personal anecdote should be viewed as sufficient evidence to contest the findings of a Cochrane Review.
3
1
37
Consensus statement: @SafeAirway principles of airway management and tracheal intubation specific to the COVID‐19 adult patient group. Now available in early view in @theMJA. All nicely formatted.
4
24
36
I can't express my enthusiasm for this paper enough. Everything you ever wanted to know about the art & science of facemask ventilation from @lowebrad.
What is your preferred hand grip position for a difficult airway?. @lowebrad and Dr Craig Lyons demonstrate the various techniques in the #BJAEducation article this month. #Airway @dastrainees @AirwayHub.
3
7
34
1️⃣ Establish ventilation . Sugammadex is not an alternative to neck rescue in CICO. Reverses NMBA but patient may still not breathe due to opioids, BZDs, induction agents, cerebral injury & it makes FM, SGA, TT & neck rescue harder. Sugammadex only an option in the Green Zone.
💢Can sugammadex save a patient? . 14 Years later, but still very to the point. 1️⃣Calculate the total needed dose before you use high dose rocuronium.2️⃣Bring enough vials to the operating room or ED or ICU before your start intubation.3️⃣Remember that you will need 16 mg/kg total.
4
10
34
@Assoc_Anaes Also need to consider strategies beyond labelling such as red plunger syringes used for NMBAs in Australia & NZ.
4
1
32
Congratulations @dr_imranahmad, @gunjeet99 & team. Fantastic program, really enjoyed it. The future of airway meetings has arrived!. #GAMC2020
0
7
34
#ExcellenceThroughCollaboration. An outstanding document by the amazing @SafeAirway team including @drdavidbrewster @DrGivasHit @precordialthump @cjgroombridge and many others.
Consensus statement: @SafeAirway Society principles of #airwaymanagement and #intubation specific to #COVIDー19 adult patient group. Out now as pre-print version on @theMJA website to help front-line clinicians. Get training!
1
7
32
Excellent article by @doctimcook in @Anaes_Journal discussing modes of #Coronavirus transmission and the role of various forms of PPE in preventing this. A great source of information to decrease anxiety and associated PPE wastage.
0
21
31
Updated @SafeAirway Consensus statement on airway management in the the COVID-19 patient group in @theMJA . Many important updates based on what we've learned just in the last 2 weeks. @drdavidbrewster @precordialthump @DrGivasHit @jgatward @cjgroombridge.
1
27
32
Difficult Airway Navigator: Innovative project to integrate diff aw documentation into EHR by @SamSchechtman at @UMichAnesthesia @umichmedicine. Incl customisable visual representation of anat aw challenges that can also be printed out & placed at bedside.
4
17
27
It would be great if the Australian government & media could get this worked up about the drug errors that occur everyday, exposing patients to risk of or actual serious harm due to look alike packaging & poorly designed electronic prescribing systems. @EzDrugID.
2
5
29
@AirwayMxAcademy 100% agree. “Difficult airway” is subjective, absolute & fixated on anatomical factors. If I intubate a morbidly obese patient on 1st pass following ramping, PreOx, ApOx using HAVL & most experienced staff was it “difficult”? No. Was airway Mx challenging/complex? Yes.
4
6
29
For info on technique for HAVL watch this virtual workshop with @gaspasser from @AirwavesLive @SafeAirway .
0
18
31
@cliffreid Lots of nuance to SGA insertion tech. If struggling, highest yield optimisations are prob jaw thrust, rotation/jiggle, laryngoscope & relaxant. But optimisations should be targeted according to whether challenges are w SGA entry, passage or seating.
1
11
31
#vDAS2021 @doctimcook: point of “No Trace, Wrong Place” isn’t to imply that oesophageal intubation is the ONLY cause of absent capnograph but rather to stress that if the capnograph trace is absent, oesophageal intubation should be EXCLUDED before moving on.
4
17
30