Vinayak Muralidhar
@DrVMuralidhar
Followers
199
Following
1K
Statuses
306
Father | Husband | Dog owner | @cds_tuhsd graduate | Dad jokes
Joined September 2019
@VedangMurthy @akshay_dinesan @RadOncTMC @docpriyamvada @drmaneesh_singh @PrachiSMehta Great study. Congratulations! Love your team’s approach to these type of practical questions.
0
1
2
@PDBrownOnc @yuvalpatelMD In theory a colleague can contour/plan for you but there are so many nuances to each case it’s hard to communicate it all without them basically repeating all the prep and thought you’ve put in. But you don’t see consults while you’re away so the next 2-3 weeks should be lighter!
0
0
1
@DavidSherMD @NiuSanford Agree it’s not really stereotaxy (in fact CBCT is more accurate than stereotaxy) but stereotactic does sound cool so I don’t mind keeping it in there. Can always invoke that language is evolving and meanings can change etc etc
0
0
1
@NiuSanford Great post. Very hard to define but you kind of know a case is SBRT if you see it. “Cancer” is similarly difficult to define—any individual characteristic is shared with at least some normal physiology.
1
0
2
@CanesDavid In my note for a case like this, I’ll often classify them as “technically unfavorable intermediate risk” as a nod to myself and others that they are UIR by the book but I really feel they are peognostically more similar to FIR.
1
0
2
@drmattmc SBRT is more humble. SABR (with “ablative” in the name) presupposes the effect. Would be like renaming CCRT to “curative chemoradiation”. Then again I think I’ve heard @BobTimmermanMD say he favors SABR so that might be reason enough to go with SABR
0
0
1
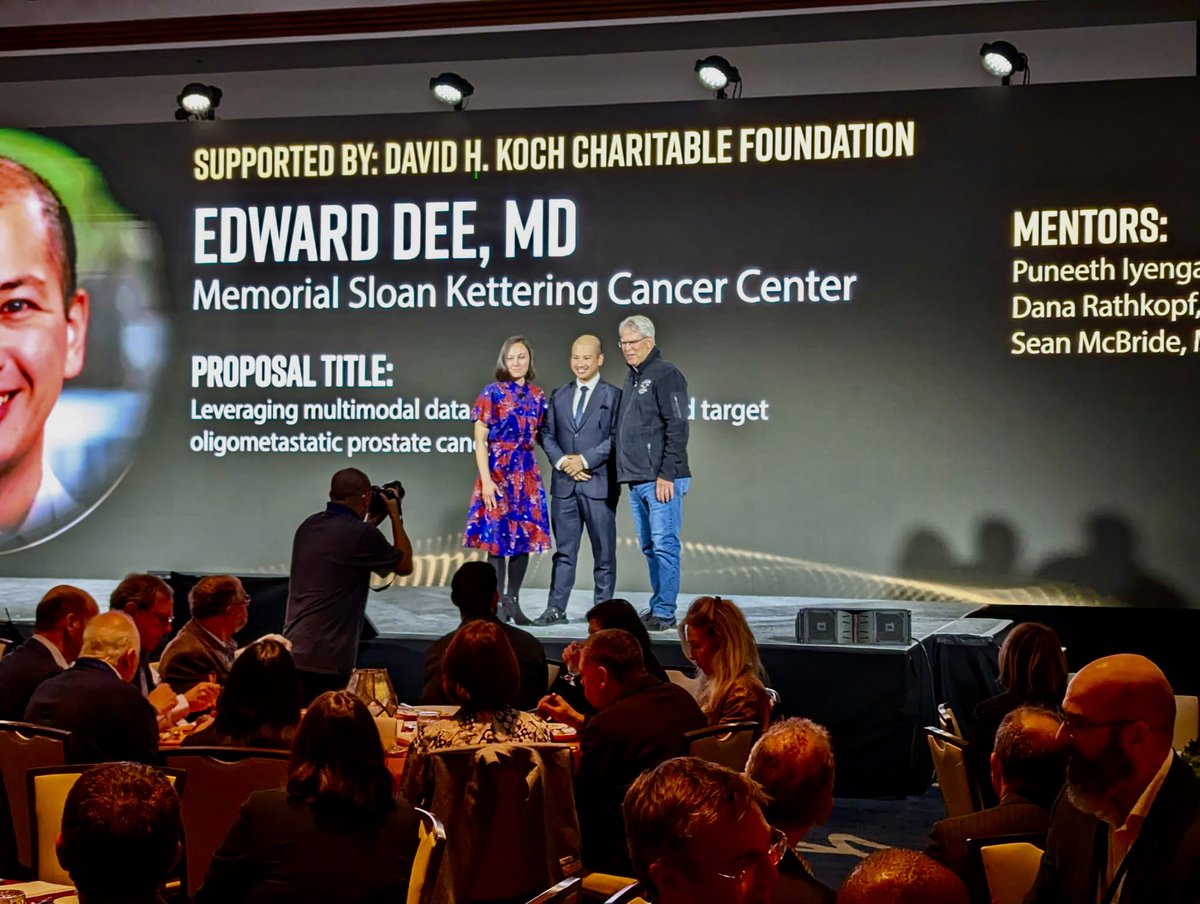
Congratulations @EChrisDee on this amazing accomplishment!! So proud to know you
Thank you @PCF_Science for the Young Investigator Award 🤩 So grateful to mentors Drs @IyengarPuneeth @DRathkopf @SeanMMcBride @DrPaulNguyen @BrandonMahal @DrVMuralidhar Dedicated to #curing #patients w #metastatic #pcsm
1
0
3
@TallAllen @AshwinShindeMD @TylerSbrt @nickva1 @NEJM @alison_tree @ICR_CTSU @EmmaHall71 @royalmarsdenNHS @DrAndrewLoblaw @cpeedell @DrTolan @ProfJOSullivan @DrSuneil_PCa @royalmarsden @Accuray @VedangMurthy @SbrtSean @SABRconsortium @gerryhanna @DrSpratticus @Mat_Guc @AmarUKishan Yes agreed. Just hoping to get clarification that that’s how it was done. I haven’t seen MRI T stage broken down into T2a vs T2b vs T2c. Usually I just say radiographic T2, mirroring the updated pathologic T stage convention
0
0
1
@AshwinShindeMD @TylerSbrt @TallAllen @nickva1 @NEJM @alison_tree @ICR_CTSU @EmmaHall71 @royalmarsdenNHS @DrAndrewLoblaw @cpeedell @DrTolan @ProfJOSullivan @DrSuneil_PCa @royalmarsden @Accuray @VedangMurthy @SbrtSean @SABRconsortium @gerryhanna @DrSpratticus @Mat_Guc @AmarUKishan @nickva1 In this table, could a patient with MRI evidence of disease involving the bilateral gland count them as T2c, hence potentially unfavorable intermediate risk if 3+4? I would typically risk stratify such a patient as cT1c/rT2, Gleason 3+4 favorable intermediate risk
1
0
0
@alison_tree @SprakerMDPhD @DrChowdharyMD Great example of why a post hoc analysis of this type of question can be flawed
0
0
1
@alison_tree @DrAndrewLoblaw @DrAPathmanathan @DrSuneil_PCa @EmmaHall71 In PACE-C, how has ADT been typically given relative to SBRT? I tend to give ADT at sim, and so on the GU013 (US trial asking a similar question), I do worry a little about the risk of the prostate shrinking between sim and the last fraction of SBRT about 3-4 weeks later
3
0
2
@5_utr Well there they may be making the choice between convenience and cure, and choosing convenience. So it’s not inconceivable they would choose convenience over a 1/10 higher chance of GU tox
1
0
0
@5_utr I agree to me it’s not as bad as GU tox but not every patient will see it that way. Some patients will choose no treatment at all compared to 20 fractions, sometimes even compared to 5 fractions.
1
0
0
@5_utr Well inconvenience is a form of harm too. The patient can choose what type of harm he prefers (GU tox or inconvenience). That’s better than the situation before PACE B when there was no choice (with known equal oncologic outcome)
1
0
0
@5_utr Wait you’re saying if the risk of GU tox had been 0% vs 1% you’d tell your patient their risk of GU is infinity times higher with SBRT?
1
0
1
@5_utr I think the relative risk is actually more misleading. The patient’s risk of a change in lifestyle/symptoms is absolute, not relative to the road not taken
1
0
1
@5_utr As someone driving to a rad onc facility every day, you probably don’t see the 15 fx difference as big. But some patients might. And you might see a higher risk of g2 GU tox as big while a patient might not. SBRT is an excellent option for patients who choose these tradeoffs.
1
0
0